What is joint cartilage ?
Cartilage is the connective tissue composed mainly of chondrocytes and collagen that covers the ends of the bones in joints. It enables the bone surfaces to slide more easily over each other thus ensuring fluidity of movement, as well as protecting the bone surface by relieving pressure and rubbing exerted during movement.
Cartilage is flexible, smooth and resistant, but is vulnerable.
- It is not innervated: cartilage degeneration is not initially noticeable. Patients are only alerted by the pain with advanced forms when other tissues are affected;
- It is not vascularized: the damaged cartilage does not heal well and the damage is sometimes irreversible, particularly in adults. The synovial fluid is a source of nutrition for the cartilage. Regeneration is possible, but slow and less effective with age.
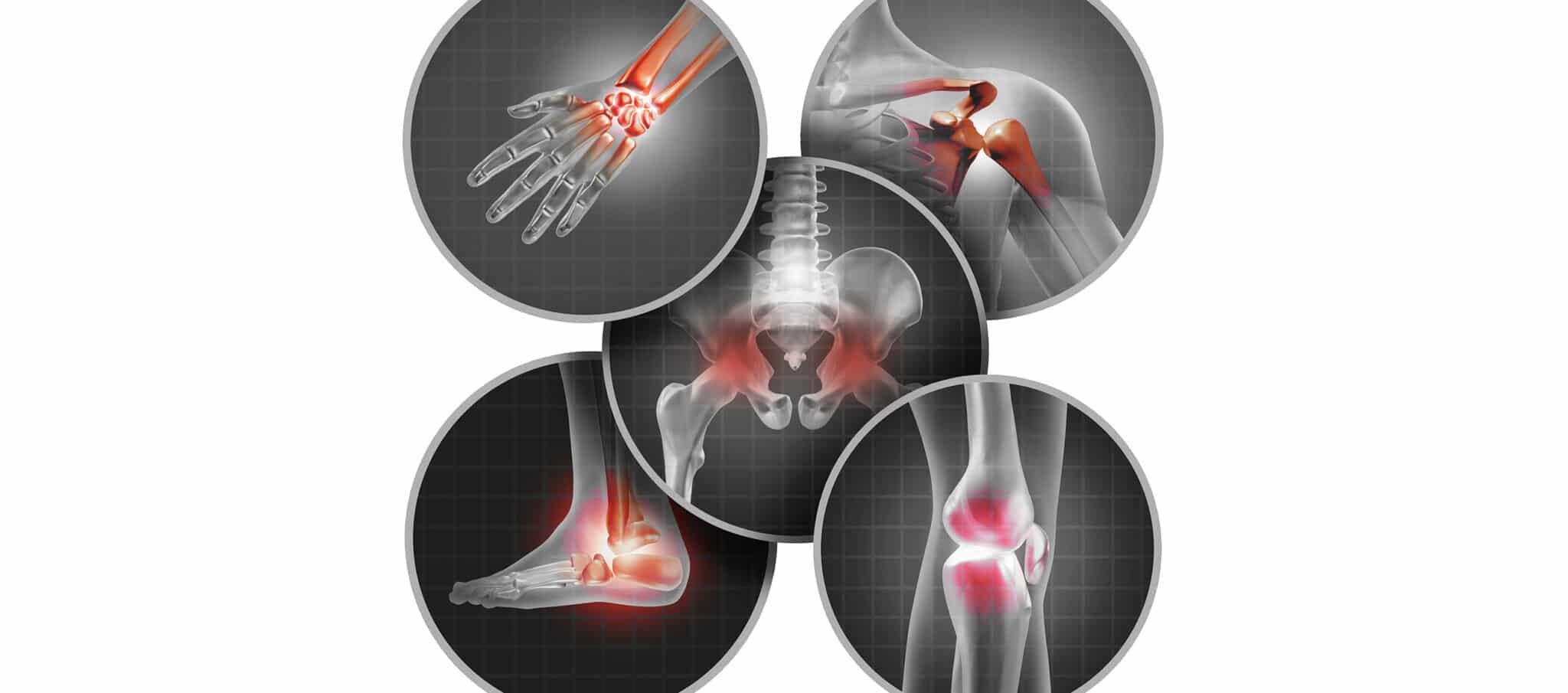
What is osteoarthritis ?
Initially, osteoarthritis is the degeneration of the cartilage and is often due to wear and tear. As the disease progresses, other tissues in the joint, such as the bone or the synovial membrane, are affected. The cartilage is exposed to significant compression and rubbing and is thus weakened, cracks, thins, and sometimes completely disappears leaving bare bone. This results in significant pain, inflammatory reactions (characterized by the secretion of too much synovial fluid, called effusion) and functional incapacity. With advanced forms, the sub-chondral bone thickens and hardens, sometimes resulting in the formation of bone outgrowths called osteophytes, which can ultimately result in clinically visible deformations.
The mechanism of cartilage wear has two origins: aging (primary osteoarthritis), and wear linked to a disorder or traumas often encountered in athletes (secondary osteoarthritis). These mechanisms can occur simultaneously.
The causes of osteoarthritis
Age
Only a small proportion of the population under 45 years suffers with osteoarthritis, and it is often related to specific activities. However, it is considered that 65 % of people aged over 65 years suffer with osteoarthritis, and this proportion increases proportionally with age. It is the primary cause of disability in the elderly.
Excess weight and obesity
This factor is implicated notably with regard to weight-bearing joints such as the knees or hips. The functional mechanism is clear: the joints are subjected to greater body mass, the cartilage is subjected to greater pressure and rubbing, and is thus more susceptible to damage caused by wear. However, some studies tend to highlight metabolic mechanisms, which could have an impact on cartilage degeneration. Indeed, overweight or obese subjects also suffer more with hand osteoarthritis, for example.
Sedentary lifestyle
The absence of physical activity frequently contributes to the onset of osteoarthritis. Indeed, sports activities, even gentle, improve muscle tone, which helps relieve the strain exerted on the joints and therefore the cartilage.
Joint overuse
Significant stimulation of the joints (repeated twisting, micro-traumas) or carrying heavy loads, whether associated with a professional occupation or intense sports activities, accelerate the onset of osteoarthritis by accentuating the pressure and rubbing exerted on the cartilage. This is more particularly observed with osteoarthritis of the lower limbs.
History of traumas and anatomical anomalies
Whatever the origin, any joint damage or malformation can lead to poor biomechanical function. When the strain exerted is no longer spread evenly throughout the joint cavity, some parts of the cartilage are exposed to too much pressure and there is a risk of accelerating the onset of osteoarthritis if the anomaly is not rectified.
Joint disorders
Some joint disorders, whether infectious or inflammatory, accelerate the onset of osteoarthritis. This is true in the case of conditions directly affecting the cartilage (e.g. chondrocalcinosis), as well as conditions linked to other joint tissue such as the synovial membrane (e.g. rheumatoid polyarthritis), the ends of the bones (e.g. ochronosis), and the ligaments or tendons (e.g. tendinitis).
Other predisposing factors
Women are much more frequently affected than men are. In addition, hereditary factors are often observed.
The symptoms of osteoarthritis ?
Pain
This symptom is generally the main reason subjects suffering with osteoarthritis consult a physician. However, as the cartilage is not innervated, pain is not strictly speaking a symptom of cartilage wear. It becomes noticeable with relatively advanced forms when other tissues are affected.
The pain is mechanical and occurs when the joint is mobilized, but is alleviated at rest. It is generally minor in the morning, increases throughout the day, and is worst in the evening. Inflammatory flare-ups occur with more advanced forms, and can lead to painful nocturnal flare-ups.
Edema
This is characteristic of knee osteoarthritis and is caused by the effusion of the synovial fluid in the joint cavity. If there is no inflammatory condition, there is generally no redness or heat.
Joint stiffness
Patients with osteoarthritis frequently describe cracking, catching or even blocking sensations, giving way or “stiffness” after a period of rest.
Functional incapacity
This is partly due to the pain, but also the disappearance of the cartilage, which impairs joint function.
Deformations
They are characteristic of the fingers and knees. With more advanced forms of osteoarthritis, bone excrescences lead to deformed joints, which contribute to stiffness and result in partial disability.
Treatment of osteoarthritis
To date, there is no curative treatment for osteoarthritis, only preventive (to prevent osteoarthritis developing or worsening) or symptomatic (to relieve the pain). With severe forms causing significant pain or disability, surgery is the only option.
Partial rest
It is essential to partially rest the joint during painful flare-ups. Sticks to relieve the lower limbs or a cervical collar can be proposed.
Weight loss
The aim is to relieve the strain on the joint to prevent its deterioration. It is also beneficial with advanced osteoarthritis as even a little loss of weight can significantly relieve pain.
Physical exercise
It must be adapted to the patient and the damage. The aim is to improve muscle tone to relieve the strain exerted on the joint. In addition, it helps with weight loss.
Adapting daily activities
Once the traumas causing the osteoarthritis have been identified, adapting the work environment or even a career change, or a change in sports activities can help ensure that the damage does not progress to severe forms.
Oral analgesics and anti-inflammatories
They are used to relieve the pain but have no incidence on the progression of the disease.
Infiltrations
When oral treatments no longer relieve the pain, the doctor can inject corticosteroids directly into the joint. In general, this provides patients with effective relief, but the number of injections is limited to avoid any potential adverse effects.
Viscosupplementation
This consists in injecting hyaluronic acid directly into the joint. This helps lubricate the joint, thus facilitating movement and decreasing the pain. However, results from recent studies concerning the efficacy of this procedure are mixed.
Surgery
When the pain and functional impairment become too severe, surgery can be proposed.
Arthroscopy : It removes the debris resulting from the degeneration of the cartilage (cause of synovial fluid effusion) that accumulates in the joint cavity, and therefore reduces inflammation.
Cartilage graft (mosaicplasty or cartilage cell graft) is the only way of recovering healthy cartilage. However, it is not suitable for all patients and is not possible when cartilage damage is very localized.
An osteotomy is a procedure that realigns a member in relation to another to ensure the even distribution of the strain exerted on the cartilage. Results are excellent with knee osteoarthritis.
Arthroplasty consists in the partial or total replacement of the damaged joint. This major operation is now extremely successful and is performed when the cartilage is totally destroyed. Patients with severe pain and disability can then return to a normal life and play numerous sports.
Arthrodesis is the surgical welding of the joint, and is a very rare operation. Nowadays, it is only performed for certain advanced forms.