
The benefits of swimming
Swimming, whether breaststroke, freestyle, backstroke or butterfly, is possible all year round, but summer is the perfect time to do more. It is a sport with numerous benefits for our physical and mental health,.
Find the latest news from Dr Philippe Paillard, orthopedic surgeon specializing in hip, elbow, knee, ankle and shoulder surgery.


Swimming, whether breaststroke, freestyle, backstroke or butterfly, is possible all year round, but summer is the perfect time to do more. It is a sport with numerous benefits for our physical and mental health,.
What is Intratissue Percutaneous Electrolysis (EPI) ? Intratissue percutaneous electrolysis or EPI isa method used to treat tendonitis and muscle injuries. This technique usesa low-intensity electric current.
What is Intratissue Percutaneous Electrolysis (EPI) ? Intratissue percutaneous electrolysis or EPI isa method used to treat tendonitis and muscle injuries. This technique usesa low-intensity electric current.

The average stay in hospital for a knee replacement is generally 5 days but now patients can stay in hospital for only 2 days or even just 8 hours. This type of surgery, known as outpatient or short-stay surgery.

What is iliotibial band syndrome? Iliotibial band syndrome (ITBS), sometimes called runner’s knee, is a recurrent condition suffered by long distance runners (marathon runners, joggers) and cyclists. This tendi.
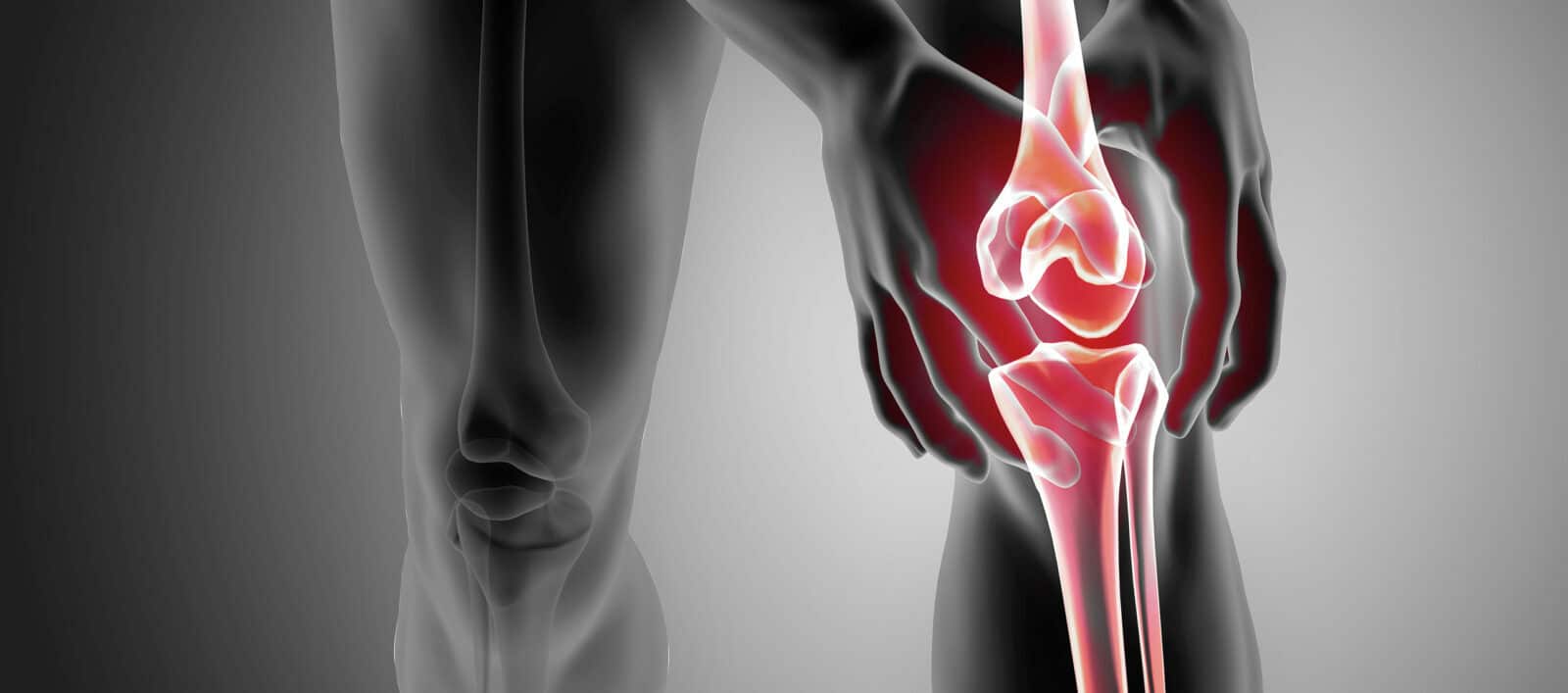
How does the knee work? The knee joint connects the femur to the tibia, and the patella, or kneecap, is located on the front of the knee. This joint comprises three compartments: medial, lateral, and anterior (.
Platelet-rich plasma (PRP) injections are being increasingly used to treat tendon, muscle, and joint conditions. Well-known among athletes, platelet injections are also being used more and more to treat symptoms.

Partial anterior cruciate ligament or ACL damage generally occurs as a result of a minor sports injury. The fibers of the medial collateral ligament are stretched but do not totally rupture resulting in laxity i.

Ankle sprains are the most common traumatic injuries sustained during sports or daily activities when there is a deficit in muscle tone, and most often damage the lateral ligament of the ankle. L’entorse du l.