Patella realignment
You have a patella dysfunction
You are going to undergo patella realignment surgery

You have a patella dysfunction
You are going to undergo patella realignment surgery
Patella realignment
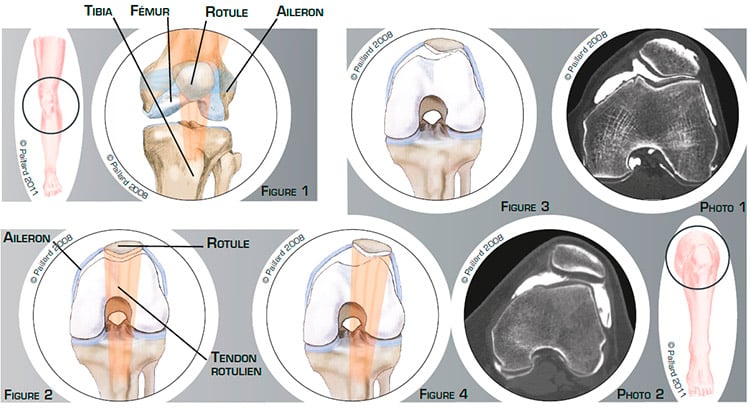
The knee is the joint between the femur and the tibia. The patella is the third bony part of the joint and is located in front. The sliding surfaces are lined with cartilage. The stability of the patella is maintained by the quadriceps tendon at the top and the patellar tendon at the bottom where it is attached to a bump on the end of the tibia called the anterior tibial tuberosity, and the medial and lateral patellar retinacula on the sides. The retinacula are like ribbons of varying elasticity located either side of the patella connecting it to the femur (figures 1 and 2).
The patella sits in the trochlea groove, which is of varying depth. The perfect fit of the patella in the trochlea groove depends on the anatomical shape, the tendons and the patellar retinacula.
A retraction of the lateral retinaculum, more or less associated with a more lateral insertion of the patellar tendon and the anterior tibial tuberosity on the tibia, results in a patella dysfunction. It can be in the form of a lateral tilt of the patella causing cartilage hyper-pressure (figure 3 and photo 1) or associated with a lateral displacement leading to poor contact of the joint surfaces (figure 4 and photo 2).
This will cause isolated pain, locking, swelling, a feeling of instability or even dislocations of the patella requiring medical treatment and physiotherapy.
The patella does not realign itself spontaneously and will progressively damage the cartilage. In this context, the natural progression is a gradual deterioration of the joint and therefore increased discomfort.
Pain which persists with the medical treatment and physiotherapy, as well as the occurrence of recurrent dislocations, raises the question of the need for surgery. The objective of the operation is to realign the patella in the trochlea groove thus relieving the pain, stabilising the patella and preventing the deterioration of the joint.
The surgery consists in realigning the patella in the trochlea groove in order to recover normal, unrestricted tracking.
Two procedures can be envisaged according to the anatomical variations and the symptoms suffered.
Lateral retinacular release is indicated in the case of a lateral tilt of the patella with a retraction of the lateral retinaculum.
This procedure is performed arthroscopically, that is, without opening the joint. Two small 5-mm incisions are made in the front of the knee. An arthroscope, or small camera, is inserted through one of the incisions to view the joint. Small instruments are inserted through the other incision to cut the retinaculum (figure 5). The patella is returned to its normal position in the trochlea groove thus reducing the excessive pressure (figure 6) and the lateral retinaculum can then heal more loosely.
If it is a dislocation of the patella
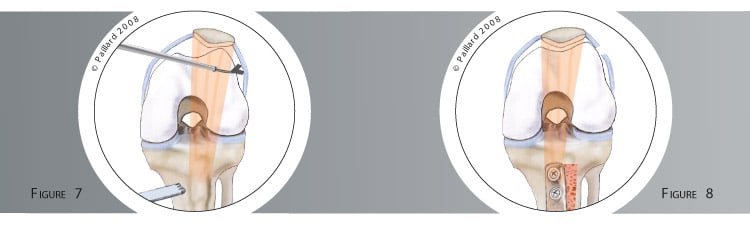
in relation to the trochlea with retraction of the lateral retinaculum and a lateral insertion of the patellar tendon and anterior tibial tuberosity on the tibia, the release of the retinaculum alone is not enough. It must be combined with a translation of the Anterior Tibial Tuberosity.

After the arthroscopic release procedure, an incision of approximately 5 cm is made in the upper part of the tibia and the anterior tibial tuberosity exposed. It is cut using a saw (figure 7), translated and repositioned in the middle of the tibia then fixed with two screws. These two procedures thus enable the repositioning and stabilisation of the patella in the centre of the trochlea (figure 8).
Patellar and trochlear cartilage damage can be treated at the same time according to their nature.
Retinacular release lasts about half an hour and requires 1 or 2 days in hospital. When it is combined with the translation of the anterior tibial tuberosity, the operation lasts about an hour and requires 3 to 4 days in hospital.
The operation can be carried out under spinal or general anaesthesia. Your anaesthesiologist will decide with you the best type of anaesthesia according to your state of health.
After the operation, the incisions are covered with a sterile dressing, which is left in place for 15 days. The pain will be managed and monitored very closely during the post-operative period, and the treatment will be adjusted accordingly.
In the case of a translation of the anterior tibial tuberosity, your knee will be immobilized and protected with a brace for the first 4 weeks to give the bone time to heal.
You will begin rehabilitation with your physiotherapist after the operation. The objective is to maintain knee flexibility and muscle mass.
If only the lateral patellar retinaculum is cut, you can start walking the next day. As the days go by, you will start walking normally. However, you should restrict your movement during the first 10 days to prevent your knee from swelling.
Driving can be envisaged after the 15th day, and you can generally return to work after the 1st month, depending on your profession; office work can be sooner. You can generally resume sports activities between the 2nd and 3rd month.
In the case of a translation of the anterior tibial tuberosity, you will have crutches to help you move around for 4 weeks so as to not to put too much weight on the knee. A brace will be used when moving around and at night for 6 weeks. Driving and returning to work can be envisaged in the 2nd month, depending on your profession; office work can be sooner. You can generally resume sports activities after the 3rd month.
In addition to the risks associated with any surgery and the anaesthetic, there are some risks specific to this surgery :
This list of risks is not exhaustive. Your surgeon can provide you with any additional explanations and will be available to discuss the advantages, disadvantages and risks of each specific case with you.
Whichever procedure is used, the locking, swelling and feeling of instability will improve rapidly after the operation. The effect on the pain may depend on the existence of underlying cartilage damage. An additional medical treatment may be required.
Complete recovery of mobility and muscle strength generally takes about 2 to 3 months.
A relapse of instability can occur during certain activities, and may require an additional procedure.
The results are however encouraging as an improvement in pain and knee function is observed in over 80 % of cases and a stabilisation of the patella in over 90 % of cases.
Laissez votre commentaire