Knee ligament reconstruction
You have a ruptured anterior cruciate ligament
You are going to undergo arthroscopic anterior cruciate ligament reconstruction
You have a ruptured anterior cruciate ligament
You are going to undergo arthroscopic anterior cruciate ligament reconstruction
Knee ligament reconstruction
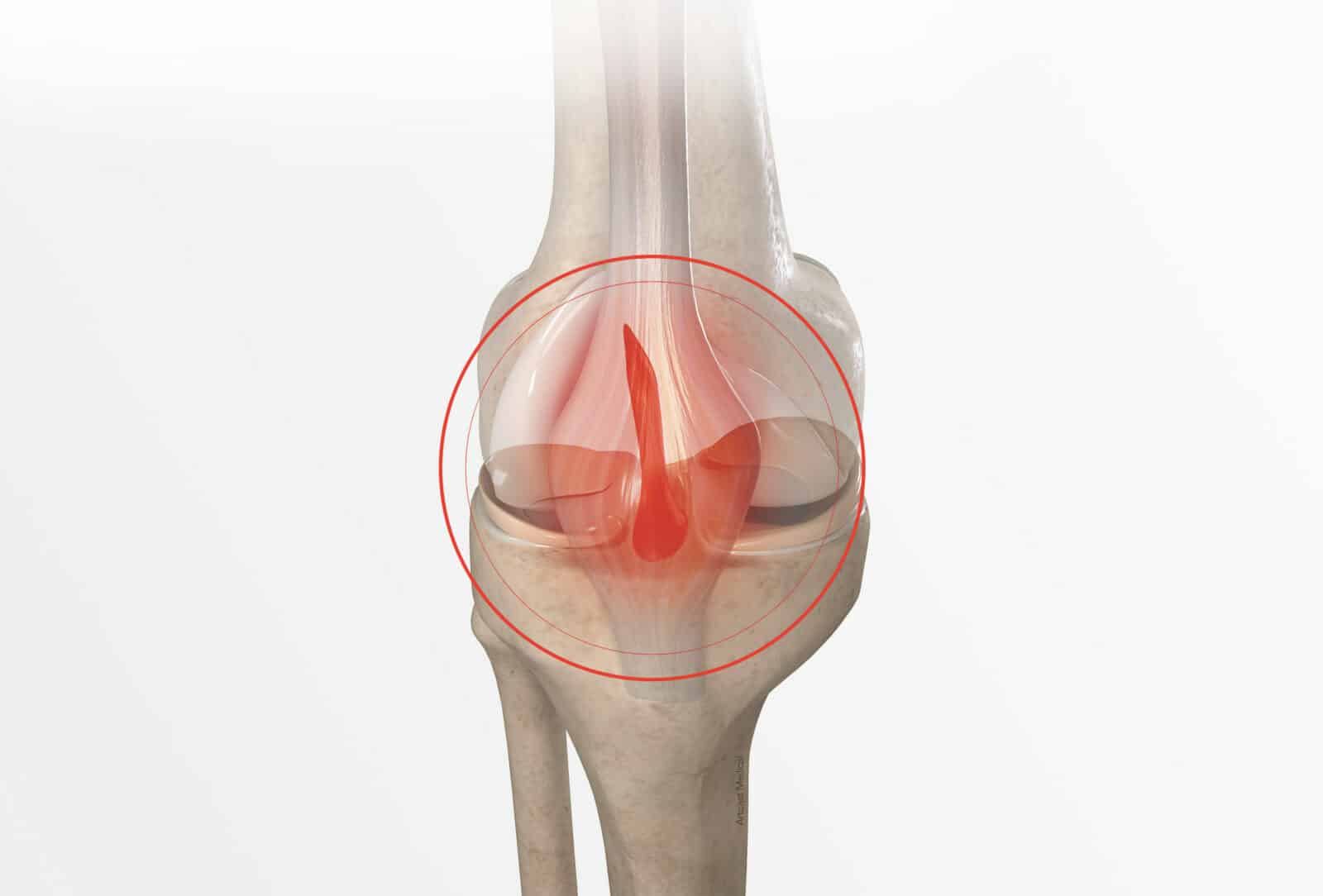
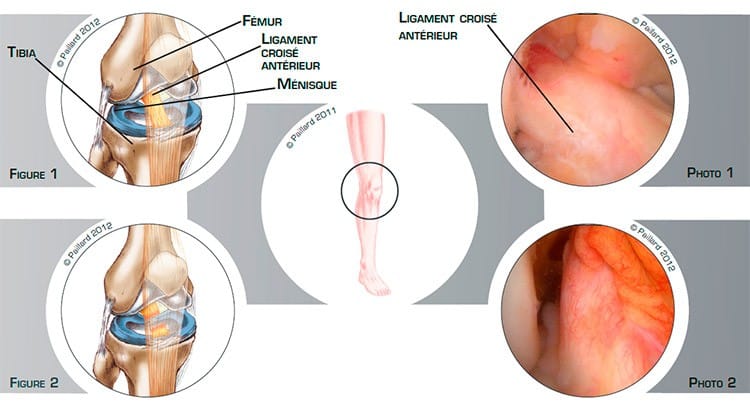
The knee is the joint between the bottom of the femur and the top of the tibia; the sliding surfaces are lined with cartilage. The menisci are small C-shaped cushions which improve the contact and act as shock absorbers between the cartilage of the femur and the tibia.
The ligaments are ribbons of varying elasticity which help maintain the stability of the knee. The anterior cruciate ligament, located inside the joint, connects the anterior part of the tibia to the posterior part of the femur. It prevents the tibia from sliding forward and stabilises the knee during rotational movements (figure 1 and photo 1).
This ligament can rupture following a trauma, causing knee instability and a locking sensation (figure 2 and photo 2). This instability is felt more during sports activities or during rotational movements of the leg.
A ruptured anterior cruciate ligament does not heal spontaneously in an effective position and the repercussions on knee stability vary from person to person.
Some sports activities and some movements cannot be achieved in the absence of an effective anterior cruciate ligament. These activities result in instability accidents which can damage the cartilage, menisci and other ligaments. In this context, the natural progression is the gradual deterioration of the joint.
The objective of anterior cruciate ligament reconstruction is to recover a perfectly stable knee so as to be able to carry out all types of activities, thus preventing cartilage or meniscal damage and the deterioration of the joint.
Anterior cruciate ligament reconstruction of the knee consists in replacing the ruptured ligament. This procedure is performed arthroscopically, that is, without opening the knee joint. Arthroscopy spares the anatomical structure and the joint can be accessed without damaging the muscles. This technique therefore has proven advantages in relation to traditional surgery, including minimal blood loss and faster post-operative recovery.
An arthroscope, or small camera, is inserted into the joint to view the ruptured ligament and assess the meniscal and cartilage damage.
Several small instruments are then inserted to carry out the surgery.
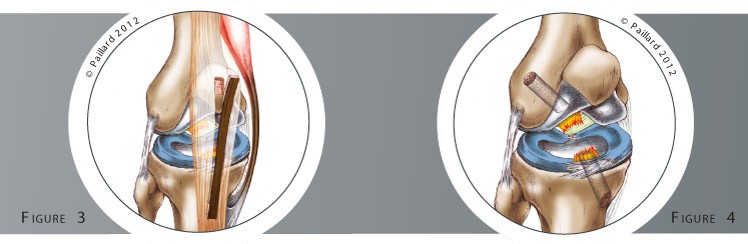
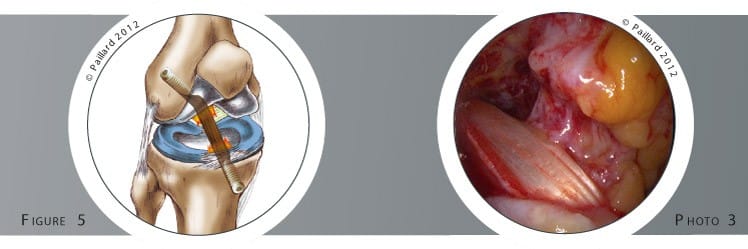
A small incision is made to remove part of one of the tendons located near the knee: the patellar tendon for the Kenneth-Jones technique or two tendons in the thigh for the hamstring technique (figure 3). This piece of tendon is used to construct the new ligament which is placed in the knee to replace the ruptured ligament. It is attached in a tunnel to the femur and in another to the tibia using resorbable screws (figures 4 and 5, photo 3).
This has little or no impact on the tendon from which a part has been removed as the tendon heals and functions almost as well as before the operation.
The meniscal lesions can be treated at the same time. A meniscal suture is carried out to maintain the integrity of the menisci as far as possible. If a lesion cannot be sutured, it is removed.
The operation lasts about 1 hour on average and requires 3 days in hospital.
The operation is carried out under regional or general anaesthesia. Your anaesthesiologist will decide with you the best type of anaesthesia according to your state of health.
After the operation, the incisions are covered with a sterile dressing, which is left in place for 10 days. The pain will be managed and monitored very closely during the post-operative period, and the treatment will be adjusted accordingly. A brace will be used to immobilize and protect your knee.
Post-operative rehabilitation can be carried out with your physiotherapist or in a rehabilitation centre. The objective is firstly to reduce the initial pain and maintain flexibility and mobility, then to recover muscle strength and sensations in the knee.
The brace will be worn for a total of 3 weeks. During the first week, the knee is kept straight using the brace. You will have crutches to help you move around so as not to put too much weight on the knee. From the second week, you will no longer need crutches and the brace will be unlocked so you can bend your knee. At the end of the third week, you can walk normally with no protection.
It is often necessary to wait a month before driving again, and you can generally return to work between the 1st and the 3rd month, depending on your profession. If you work in an office, you may be able to return to work sooner after the operation.
You will be able to resume sports activities with no twisting (swimming, cycling, running) in the third month. It will be necessary to wait for 6 months before resuming all sports, and another 1 or 2 months to recover all your natural reflexes and to return to competition.
In addition to the risks associated with any surgery and the anaesthetic, there are some risks specific to this surgery :
This list of risks is not exhaustive. Your surgeon can provide you with any additional explanations and will be available to discuss the disadvantages and risks of the operation with you.
The pain, locking and feeling of instability should disappear rapidly after the operation. Complete recovery of mobility and muscle strength general takes about 3 to 6 months.
The condition of the muscles is a major element to be taken into consideration before pushing the knee to the limit, in particular in sport. The replaced ligament is no better than the original ligament and can rupture again. It is therefore necessary to be careful given the risks posed by sports that involve twisting of the knee such as tennis or football.
The results of this technique are nevertheless very encouraging as a stable knee with functional improvement is obtained in over 90 % of cases. The risk of cartilage and meniscal deterioration is lower with a stable knee.
Laissez votre commentaire