Revision knee replacement
You have a loosening of the knee prosthesis
You are going to undergo revision total knee replacement

You have a loosening of the knee prosthesis
You are going to undergo revision total knee replacement
Revision knee replacement
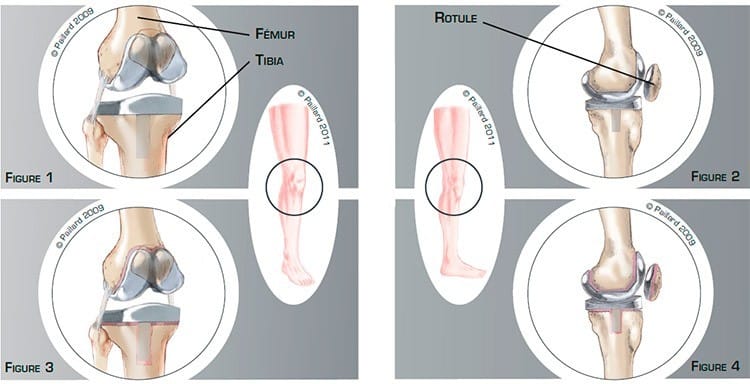
The total knee implant is made up of four components: the femoral component, the tibial component, the patellar component and an intermediary plastic component which provides a slick surface between the femur and the tibia (figures 1 and 2).
The stability of the implant is ensured by the ligaments, which are like ribbons of varying elasticity connecting the femur to the tibia. The functioning of the implant is ensured by all the tendons connecting the muscles to the bone, particularly the extensor mechanism formed by the quadriceps, the patella and the patellar tendon.
Over time, the intermediary component wears and the fixation of the implant to the bone deteriorates. Little by little the cement between the implant and the bone deteriorates. This leads to the progressive loosening of the implant resulting in mobility in relation to the bone (figures 3 and 4). Causes other than natural wear, such as a chronic infection or poor positioning of the implant, can result in this developing more rapidly after the operation.
The loosening will cause pain, limping, even a deformation of the limb, as well as stiffness, progressively decreasing the functional possibilities of the implant.
The wear and loosening of the implant will get increasingly worse, causing greater bone pain. The bone around the implant gets thinner and thinner and may fracture.
All these phenomena are responsible for an increasingly painful discomfort. An x-ray, scan or bone scintigraphy will confirm the diagnosis. Once the diagnosis has been confirmed, the implant must be changed.
The objective of the operation is to prevent the deterioration of the bone as early as possible and thus relieve the pain, recover mobility and return to normal walking.
The objective of the operation is to remove the old implant and replace it with a new one.
In general, the scar used for the first replacement is used. A passage is then created behind the patella to gain access to the implant.
After removal of the faulty implants, all the debris due to wear is cleaned. The healthy bone is cut again, then the femur, tibia and patella are prepared to receive the prosthesis (figure 5).

According to the bone destruction, metal wedges fixed to the implant, or even a bone graft, may be necessary to achieve the correct positioning of the new implant.
The fixation of the implant is reinforced by stems in the femur and tibia (Figures 6 and 7).
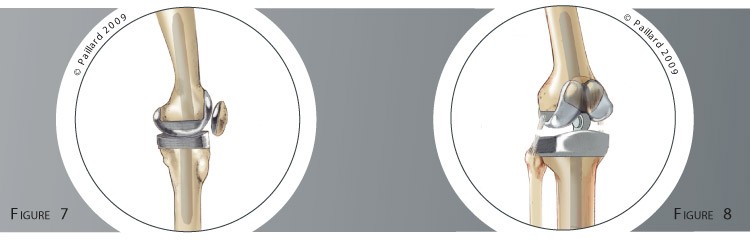
If the ligaments that ensure the stability of the implant are affected, or in the event of massive bone destruction, a “hinge” prosthesis will be used. The femoral and tibial components are connected to ensure the stability of the knee. This increases the pressure on the bone and requires long stems in the femur and tibia to ensure the fixation of the implant in the bone (Figure 8).
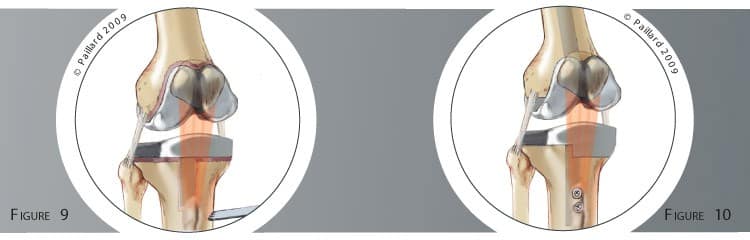
In some cases, it may be necessary to cut the anterior tibial tuberosity where the patellar tendon is attached to move the patella aside and obtain a good view for the operation (figure 9). In this case, it will be reattached at the end of the operation using two screws (figure 10).
If the loosening is linked to a chronic infection, a period of approximately 6 weeks is often required between the removal of the old implant and the placement of the new one. During this period, a Spacer, or temporary implant, is fitted to leave the bone time to heal with antibiotics.
The operation lasts about 2 to 3 hours on average and requires around 7 days in hospital.
The operation can be carried out under spinal or general anaesthesia. Your anaesthesiologist will decide with you the best type of anaesthesia according to your state of health.
After the operation, the incisions are covered with a sterile dressing and a brace is worn. The pain will be managed and monitored very closely during the post-operative period, and the treatment will be adjusted accordingly.
The physiotherapist will get you up the day after the operation and help you to walk. Walking sticks will be useful during the first few days, but will be progressively abandoned. You can go up and down stairs within 3 days. It is often necessary to go to a rehabilitation centre after the operation. The objective is firstly to reduce the initial pain and maintain flexibility and mobility, then to recover muscle strength and sensations in the knee.
Driving can be envisaged after the 1st month, and you can generally return to work after the 3rd month, depending on your profession; office work can be sooner.
If the anterior tibial tuberosity is cut, the brace will be kept for 6 weeks, which will delay any return to normal activities by a few weeks.
In addition to the risks associated with any surgery and the anaesthetic, there are some risks specific to this surgery :
This list of risks is not exhaustive. Your surgeon can provide you with any additional explanations and will be available to discuss the advantages, disadvantages and risks of each specific case with you.
The results of this technique are very encouraging as an often spectacular disappearance of the pain along with a rapid recovery of mobility and muscle strength are observed. Normal walking with no limping is generally obtained during the 2nd month.
Even if many patients forget they are wearing an implant, it is preferable to avoid physical work and violent sports as these activities can increase the wear and decrease the lifespan of the prosthesis despite the use of new, more resistant materials. Some activities like cycling, swimming, golf or walking are possible, and even recommended, whereas care should be taken with skiing, tennis and jogging.
The average lifespan of a knee replacement is about 20 years. With the progress in the materials used today, we hope that the results and the longevity will continue to improve.
Laissez votre commentaire