Knee cartilage surgery
You have cartilage damage
You are going to undergo knee cartilage surgery
You have cartilage damage
You are going to undergo knee cartilage surgery
Knee cartilage surgery
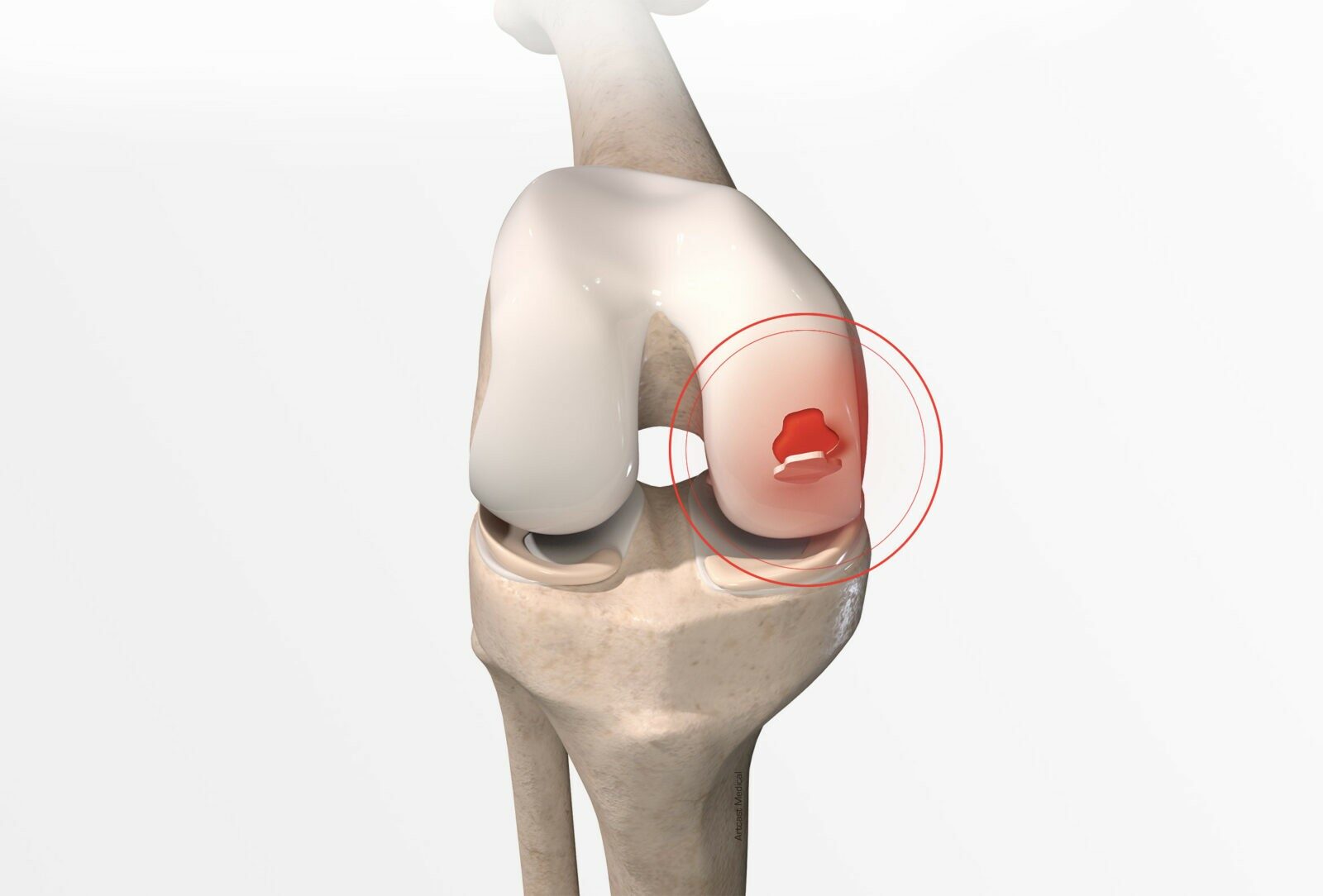
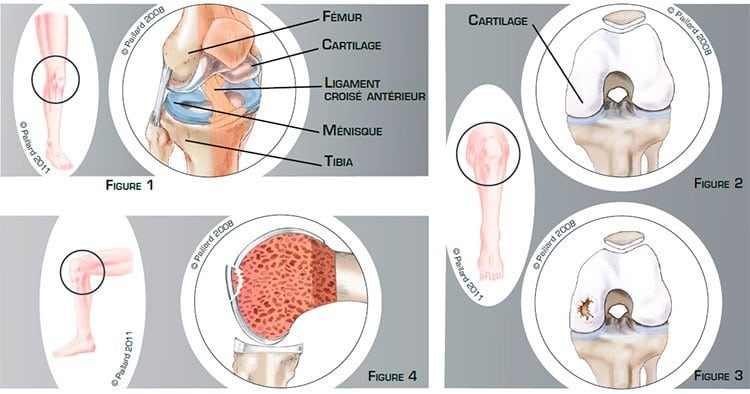
The knee is the joint between the bottom of the femur and the top of the tibia. The joint surfaces are lined with a thin layer of cartilage 1 to 2 mm thick which allows the bones to glide smoothly over each other, reducing the friction and absorbing the pressure on the bone. The menisci are small C-shaped cushions between the cartilage of the femur and the tibia which improve the contact and act as shock absorbers. Ligaments are ribbons of varying elasticity which help maintain the stability of the knee (figures 1 and 2).
Cartilage damage can occur following a blow, recurrent minor traumas, or due to a growth imperfection. The damaged cartilage comes away from its natural position alone or with a small piece of underlying bone (figures 3 and 4). It can come away partially creating a flap, or completely leaving a fragment that can move around the joint. The area of damaged cartilage can vary in size and depth.
Cartilage damage can cause pain, locking, swelling and sometimes joint weakness, thus restricting walking and other activities. Ligament or meniscal damage can be associated with and participate in the symptomatology.
The capacity of cartilage to repair and regenerate itself is very limited. A cartilage defect does not repair itself spontaneously, a partially detached lesion does not heal itself and a free fragment can get stuck between the joint, damage the healthy cartilage and eventually lead to its deterioration.
A small lesion can initially be treated medically. Surgery will be proposed in the case of a symptomatic flap or fragment, or a major cartilage defect. The objective of the operation is to restore a uniform sliding surface to relieve the pain, locking and swelling, and enable a return to normal walking and activities, thus preventing the progressive deterioration of the joint.
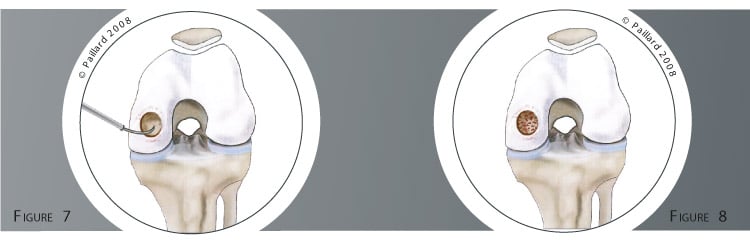
Cartilage surgery concerns localised lesions. It aims to reattach or extract a partially or completely detached lesion. It also treats the zone of the defect by cartilage grafting or stimulating cartilage repair.

In the case of a deep, broad lesion in the form of an osteochondral flap or intra-articular fragment, reattachment can be considered to enable healing. After repositioning the fragment in its original site, it is fixed with a screw to enable the homogenous reconstruction of the cartilage surface (figure 5). In the case of a shallow lesion, the chances of healing are minimal. The lesion is excised and the edges are rectified (figure 6).
If the cartilage defect is small and superficial, nothing else is done.
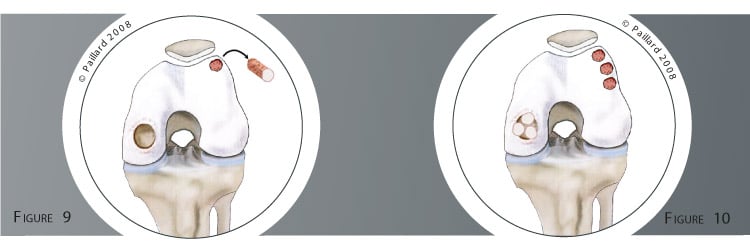
In the case of a more extensive cartilage defect, two procedures are possible to repair the defect according to its position and extent :
Cartilage surgery is performed arthroscopically or an incision is made in the front of the knee. Arthroscopy consists in making two small 5-mm incisions in the front of the knee. An arthroscope, or small camera, is inserted through one of the incisions to view the joint, and in particular the damaged cartilage. Small instruments are inserted through the other incision to carry out the surgery.
Arthroscopic surgery is often used for cartilage reattachment as well as the microfracture technique. The operation lasts about half an hour and requires 1 or 2 days in hospital. The mosaicplasty technique often requires an incision in the front of the knee. The operation lasts about an hour and requires 3 or 4 days in hospital.
The operation is carried out under regional or general anaesthesia. Your anaesthesiologist will decide with you the best type of anaesthesia according to your state of health.
After the operation, the incisions are covered with a sterile dressing, which is left in place for 10 days. The pain will be managed and monitored very closely during the post-operative period, and the treatment will be adjusted accordingly.
You will begin rehabilitation with your physiotherapist after the operation. The objective is to maintain knee flexibility and muscle mass.
In the case of a reattachment or mosaicplasty, you will have crutches to help you move around for 6 weeks so as not to put too much weight on the knee.
Driving as well as returning to work can be envisaged in the 2nd month, depending on your profession; office work can be sooner. You can generally resume gentle sports activities such as cycling and swimming after the 3rd month.
In the case of microfractures, the non weight-bearing period is 3 weeks. Driving as well as returning to work can be envisaged in the 1st month, depending on your profession; office work can be sooner. You can generally return to gentle sports activities such as cycling and swimming after the 2nd month.
Whichever technique is used, it is necessary to wait 4 to 6 months before a full return to all sports activities.
In addition to the risks associated with any surgery and the anaesthetic, there are some risks specific to this surgery :
This list of risks is not exhaustive. Your surgeon can provide you with any additional explanations and will be available to discuss the advantages, disadvantages and risks of each specific case with you.
Whichever procedure is performed, the locking, swelling and instability will disappear rapidly after the operation.
The healing of fixed osteochondral fragments varies from 75 % to 90 %; post-traumatic lesions have a greater chance of healing.
Regarding the microfracture technique, the improvement in cartilage function and condition is about 80 % in the case of an isolated cartilage lesion.
Regarding mosaicplasty, moderate discomfort around the harvesting site is observed in about 15 % of cases. Nevertheless, the results remain very encouraging as good results are obtained in nearly 90 % of cases when located on the femur, 85 % of cases when located on the tibia and 80 % for the patella.
Laissez votre commentaire